Transverse Myelitis
What is transverse myelitis?
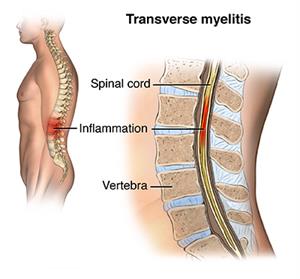
Transverse myelitis is a neurological condition. It happens when the spinal cord becomes inflamed. This inflammation can damage myelin, the insulating material that covers your nerves. Loss of myelin often leads to spinal cord scarring that blocks nerve impulses and results in physical problems.
Transverse myelitis is a relatively rare disease. It occurs most often in children ages 10 to 19 and in adults ages 30 to 39. But it can happen at any age, and to any gender or race.
What causes transverse myelitis?
In some cases, the exact cause of transverse myelitis is unknown. In other cases, the inflammation that leads to transverse myelitis can result as a side effect of a number of other health problems, such as:
Transverse myelitis can also be a warning sign of multiple sclerosis. But this is rare. Since some people with transverse myelitis have autoimmune diseases, such as lupus, some healthcare providers believe that transverse myelitis may also be an autoimmune disease. Finally, some cancers can trigger an immune response that leads to transverse myelitis.
What are the symptoms of transverse myelitis?
The symptoms of transverse myelitis can develop over several hours or days, or over a longer period of 1 to 2 weeks. These are possible symptoms:
-
Back or neck pain
-
Weakness in arms or legs
-
Abnormal feelings in the legs, such as burning, tingling, or pricking
-
Loss of bladder or bowel control
-
Heightened sensitivity to touch
Where in the body these symptoms occur depends on what part of the spinal cord is inflamed. People with inflammation in the neck typically feel symptoms from the neck down. Inflammation in the middle of the spine can cause symptoms from the waist down.
How is transverse myelitis diagnosed?
If you suspect that you have transverse myelitis, your healthcare provider will likely review your medical history and do a complete physical exam. Because transverse myelitis can be caused by a number of treatable conditions, your provider may want to test for some of those diseases. Imaging tests that may be done are MRI or CT scans.
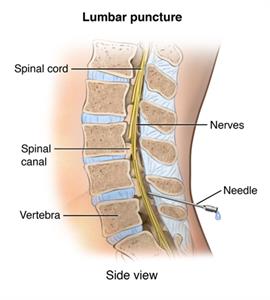
Blood tests and a lumbar puncture (spinal tap) may also be done to rule out other diseases or causes for transverse myelitis. A lumbar puncture is a procedure that uses a needle to get a small sample of cerebrospinal fluid from the spinal cord for testing.
 |
| PNerv_20140304_v0_002 |
If all potential underlying causes of transverse myelitis have been ruled out, it is called idiopathic.
How is transverse myelitis treated?
No effective cure currently exists for transverse myelitis. But there are treatments to prevent or reduce permanent neurological problems. Treatments focus on relieving the inflammation and or infection that causes the symptoms. Some people might need to be hospitalized at first if the symptoms are bad enough. High doses of steroids are used to suppress the activity of the immune system and to decrease swelling and inflammation. Your healthcare provider may also recommend pain-relieving medicines like ibuprofen or acetaminophen, immune-suppressing medicines, and specific medicines that target nerve pain.
If steroids don’t relieve the symptoms of transverse myelitis, your provider may try a procedure called plasma exchange therapy (plasmapheresis). This procedure exchanges the plasma in your blood with special fluids that remove harmful antibodies and proteins from the blood that are causing the inflammation.
Depending on the type and severity of the effects of transverse myelitis, you may need short- or long-term physical therapy. A period of specialized in-patient care in a rehabilitation facility may be necessary.
Living with transverse myelitis
The long-term effects of transverse myelitis vary among people. About 1/3 of people with transverse myelitis have full or near-full recovery, with most of their symptoms gone. Another third have fair recovery, retaining some of their symptoms. The last third recover poorly and have major physical disabilities.
When recovery from transverse myelitis occurs, it often starts from 2 to 12 weeks after you first have symptoms. It can take up to 2 years. Most people will only have a single episode of transverse myelitis. But a few people may have a recurrence.
Some people who get transverse myelitis are left with permanent physical disabilities, such as muscle stiffness, loss of bowel or bladder function, muscle weakness, or even paralysis. If you have any of these impairments, physical therapy will likely be a very important part of your treatment. In this treatment, specialists will work with you to maintain or increase your strength, improve your coordination, and help you gain more control over bladder and bowel functions.
Another type of therapy is occupational therapy. This helps you learn new ways of independently doing everyday tasks, like bathing, dressing, and preparing meals in spite of your new physical limitations.
Finally, some people with physical disabilities often feel sad or depressed. If this happens to you, your provider may recommend that you see a mental health provider. Antidepressants and psychotherapy, or “talk therapy,” can help in dealing with depression, stress, and a wide range of emotions.
When should I call my healthcare provider?
Some people recover fully from transverse myelitis within a few months or years. But others might continue to have long-term problems. Talk with your healthcare provider about when you need to call them.
Your healthcare provider will likely advise you to call them if any symptoms you are having become worse, including weakness, numbness, or other changes in sensation, or changes in bladder or bowel control.
People who have serious long-term effects from transverse myelitis, such as paralysis or loss of bladder or bowel control, can also develop a number of other complications. Your provider might advise you to call if you have problems, such as:
-
Skin sores or infections
-
Trouble breathing ( Call 911)
-
Fever or other signs of infection
-
Trouble urinating regularly or having severe constipation
-
Severe muscle cramps or spasms
-
Increasing pain
Key points about transverse myelitis
-
Transverse myelitis is an inflammation of the spinal cord. The exact cause is often not known. But it sometimes happens after infections or in people with autoimmune diseases.
-
Common symptoms are back or neck pain, weakness or sensation changes in the arms or legs, or loss of bladder or bowel control.
-
Treatment with steroids or other medicines doesn't cure transverse myelitis. But it might relieve symptoms.
-
Some people recover fully, while others might have minor or more serious long-term problems.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells you.
-
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
-
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your healthcare provider if you have questions.